Following second patient death, Duchenne muscular dystrophy families deserve answers about Elevidys
This article originally appeared on www.statnews.com, written by Christine McSherry—a registered nurse and founder of the Jett Foundation—on June 18, 2025.
On Sunday at 1 a.m. Eastern time, an announcement went out from the first-generation gene therapy company for Duchenne muscular dystrophy: A second patient who had been treated with Elevidys has died.
This second family said yes to hope, yes to science, yes to the risk, and is now grieving the irreversible outcome of an irreversible drug. Others who also said “yes” are living with consequences from adverse events that we still don’t fully understand: cardiac complications, thrombocytopenia, nausea, vomiting, and elevated liver enzymes.
These families — our families — deserve more.
I know firsthand how difficult it is to make decisions about a cutting-edge treatment, to balance the risks and potential rewards. My son Jett, the third of my five children, was diagnosed with Duchenne in 2001 at the age of 5. In 2012, I activated an exploratory qualitative program to better understand meaningful benefits that were being seen in Sarepta’s study of eteplirsen. I found that patients were benefiting from eteplirsen but, as with the disease, in heterogeneous ways that were not being captured by the more clinician-directed traditional assessments. Eteplirsen, now Exondys 51, was approved by the FDA in 2016.
Nearly 10 years later, the landscape has changed fundamentally. I am overwhelmed by the promise of gene therapy. We need to protect that promise — not by slowing innovation or fast approvals and access to life-changing medications, but by making the system work better. That begins with data, safety, and respect for those who took the biggest risk.
Duchenne muscular dystrophy is a rare muscle-wasting condition that causes muscle weakness, loss of mobility, and early death in mostly boys and young men. There are girls also with Duchenne, though they are much more rare.
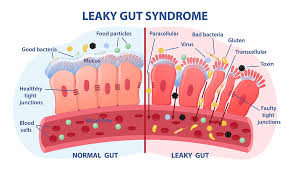
Elevidys uses a disabled virus to insert a replacement gene for producing dystrophin — the protein missing in those with Duchenne — into patient cells. The cost of the one-time infusion is $3.2 million.
The sponsor, Sarepta Therapeutics, received accelerated approval in June 2023 from the Food and Drug Administration for the use of Elevidys in ambulatory boys ages 4 and 5 years old. On June 20, 2024, Peter Marks, then the director of the FDA’s Center for Biologics Evaluation and Research, broadened the approval of Elevidys to traditional full approval for boys 4 and older and continued accelerated approval for non-ambulatory patients 4 and older.
In mid-June, Sarepta reported that more than 900 patients have received Elevidys globally, leading to more than $800 million in revenue.
We need to acknowledge just how agonizing these decisions are — and were — made by families in our community. Elevidys gave to the Duchenne community so much hope, but also risk. Decisions to participate in a clinical trial or access the commercial drug are not made on paper. They are made in private moments of fear, love, and hope by caregivers and patients who are living with a life-altering and life-limiting disorder.
But the reality is, patients who are treated — ambulatory and non-ambulatory alike — are at risk for serious complications and, sadly, death.
And while Sarepta brought us hope, it has also silenced concerns, has not fully disclosed adverse events, and appears to be operating in the best interests of its investors, not patients and families. Many of us find that we get our most reliable information from each other, from social media, where people share their experiences with Elevidys.
The FDA created the Adverse Event Reporting System (FAERS) dashboard for good reason. According to the FDA website, the purpose is to expand FAERS data access so that the general public can search for information related to human adverse events reported to FDA by the pharmaceutical industry, health care providers, and consumers. It helps us understand the risks associated with medications. The data is the responsibility of several stakeholders, including the sponsor.
However, information is missing from the Elevidys data, including patients’ ages and weight. That’s important because many in the Duchenne community want to understand if these deadly complications exist only in patients who are no longer ambulatory. Knowing a patient’s age can be extremely useful. In addition, during an investor call and update Monday morning, the CEO said that there was no evidence to also halt distribution of Elevidys for ambulatory participants.
But the FAERS dashboard confirms what the Duchenne community is reading on social media pages: Ambulatory boys have significant adverse events, including elevated liver enzymes that require complex, urgent, multidisciplinary medical care. Has the bar now been set so that only death triggers a serious evaluation of the safety of a new, irreversible gene therapy? These patients are undergoing days to weeks of multiple hospitalizations, high doses of IV steroids, rounds of intravenous immunoglobulin treatment, and when all that fails or is simply not enough, months of sirolimus, also known by the brand name Rapamune, a powerful immunosuppressant drug primarily used in renal transplant patients to help prevent their bodies from rejecting the new organ.
Given the pain, uncertainty, and expense of the treatment, we should be able to get information from the many conferences that we attend, the FAERS dashboard, and real-time communication with clearly written updates from the sponsor to help the community make educated choices. The burden of clarity, transparency, and proactive communication should fall on the sponsor — not the families.
But instead, we are stuck with social media. Caregivers of boys treated with Elevidys are sharing a growing volume of anecdotal safety and outcome data. These real-world reports — often posted out of desperation or in search of support — offer early insight into how the therapy is being experienced outside the tightly controlled clinical trial setting. But the leadership at Sarepta has not even acknowledged this outpouring of information. Clearly, the system is broken.
Looking ahead, I believe the next generation of gene therapies will bring more promise, more safety, and better efficacy. We will have better vectors, and sponsors will provide broader data. I firmly believe accelerated approval for drugs that treat rare diseases is essential, and that those drugs should use this pathway to bring therapies to patients and families as quickly as possible — and I don’t believe that needs to be years away.
But to make that vision happen, and to ensure families feel equipped to make hard decisions, we need to see changes.
That means mandatory confirmatory studies that collect real-world evidence. In addition, the sponsor and policymakers need to take responsibility to ensure all data, good or bad, is entered into the FAERS system accurately and completely — or else they must create a better system. The system should push that information proactively to our physicians, rather than requiring them to look it up themselves. The FAERS dashboard should be a mandatory resource, and there should be timely and accurate documentation — not haphazard data entry with no accountability. Irreversible treatments require a central, public repository of adverse events, interventions, and easy-to-understand multidisciplinary-guided access to complex multisystem protocols for when things do not go as planned.
We need multidisciplinary protocols with input from hepatologists, nephrologists, transplant experts, and those who have had prior experience with gene therapy. Furthermore, our neuromuscular doctors need to be supported fully. They were not necessarily trained in acute liver failure; they are not transplant physicians. They are the experts we count on daily for care of Duchenne — not liver disease.
We need FDA rigor that does not slow innovation but ensures a system with easy-to-understand informed consent and mandated post-market follow-through. And if there is failure, there need to be consequences. Regulators must require better transparency and tighten safety oversight. Policymakers must ensure that those who say yes to clinical science and rely on an “approved” commercial drug are honored with more than thoughts and prayers. They deserve action and reform.
Our community deserves these higher standards, and it is the sponsors who must meet them with partnership — not dictatorship — with our community.
Elevidys’ current label does not reflect the severity of what is happening. There should be a black box or at least a more rigorous safety information on the label so physicians know how to treat these patients.
Families are mourning. Those who said yes are terrified. We all are. The most respectful tribute is to fix this system — worthy of the courage our families have shown.
Those families, and those no longer here, deserve a drug development system that matches their bravery with integrity.